charles bonnet syndrome treatment
/charles-bonnet-syndrome-symptoms-causes-diagnosis-treatment-4174057-5c04749146e0fb00012cd0fe.png) Charles Bonnet Syndrome: Symptoms, Causes, Diagnosis, and Treatment
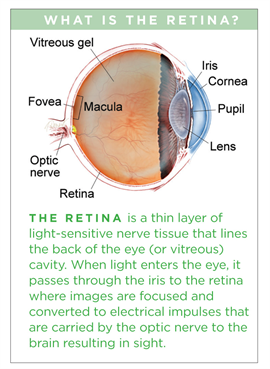
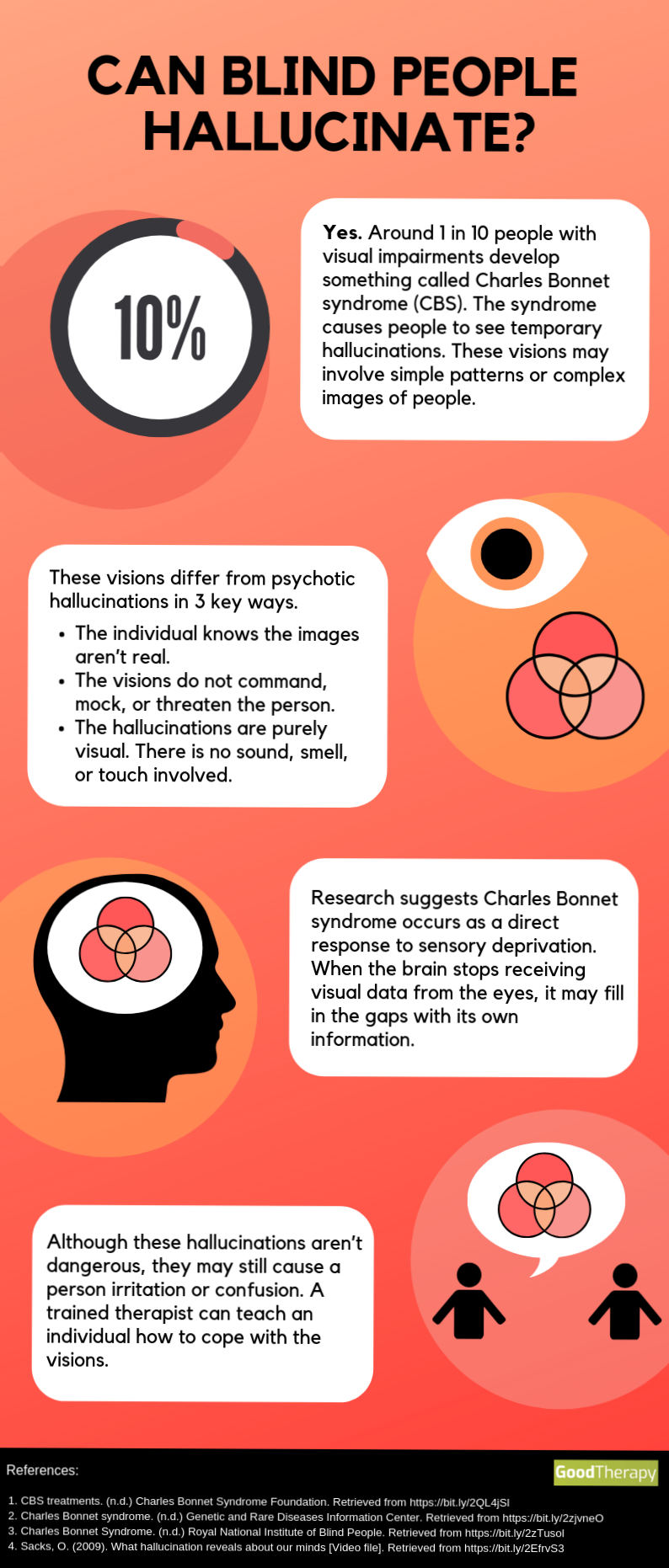
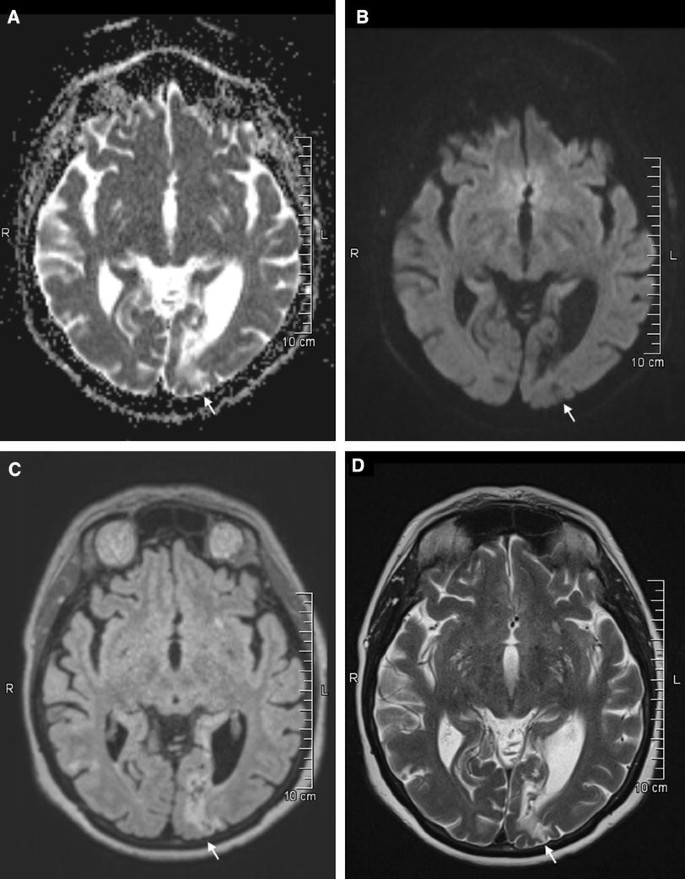
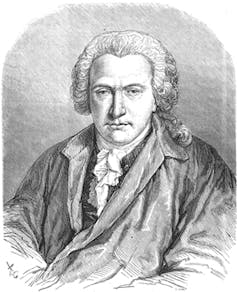
Charles Bonnet Syndrome: Symptoms, Causes, Diagnosis, and TreatmentWarning: The NCBI website requires JavaScript to operate. Charles bonnet Syndrome, management with simple behavioral technique Baba Awoye IssaDepartment of Conduct Sciences, University of Ilorin, PMB 1515, Ilorin, Nigeria Abdullahi Dasliva YussufDepartment of Conduct Sciences, University of Ilorin, PMB 1515, Ilorin, Nigeria Abstract Charles Boncognitiva Syndrome is presented in individuals with normal visual impairment, This report describes a condition of vivid visual hallucination (phantom images) in a 85-year-old conscious man who had been blinded by the progressive bilateral glaucoma deterioration. This common condition, but rarely reported, was handled by the behavioral approach of repeated blinking, intermittent eye closure, and reassurance. While emotional, humor and cognitive disorders need to be discarded, the condition, though terrifying the afflicted, is benign and remedial with a simple, inexpensive approach. Health workers who manage people with terminal blindness should always ask for the presence of hallucinations of their patients to prevent a preventable anguish resulting from misperception without visual stimulation. Introduction In 1769, Charles Bonnet described a syndrome in which vivid and complex visual hallucinations occurred in his 87-year-old psychologically normal grandfather who was almost blind to the bilateral cataract.[,] The condition was given the name of Charles Bonnet (CBS) syndrome by Mossier in 1967.[] Although the phenomenon does not occur only in the elderly with visual impairments, most affected people are elderly with visual disabilities.[] Cataracts, age-related macular degeneration or damage to other areas of the visual path may be involved.[,] While the etiology of the syndrome is not clearly understood, hallucinations in CBS are considered as "a phenomenon of liberation" secondary to the deformation of the cerebral cortex, analogous to that seen in the syndrome of the ghost member.[,] During normal vision the information received from the eyes actually prevents the brain from creating its own images.[] In the blindness the information that comes to the brain is significantly reduced. The brain sometimes fills these gaps by releasing new images of fantasy, old patterns or images that it has stored, so hallucinations.[–] The hallucinations and interpretations of the experience could scare the afflicted. [] The prevalence of CBS varies between 0.4%[] and 40%.[] The actual prevalence has been hindered by the non-representation of this disorder, which could be due to the problems of disclosure for fear of being mentally ill labeled. CBS should be differentiated from other causes of visual hallucination such as organic brain disorders and degrading diseases, substance disorders, schizophrenic disorders and mood disorders. Unlike patients with mental disorders, virtually all patients with CBS retain the perception of the unreal nature of their hallucinations.[] A careful history, physical examination and mental examination will distinguish CBS from these other differential diagnoses. No specific treatment for CBS. Although antidepressant anticonvulsants have been used for CBS with good effect in previous reports,[,] the effectiveness of these drugs in treatment is somewhat questionable and must be reserved for those who have high levels of anguish and have not responded to conventional intervention.[,] The treatment approach would also depend on other physical or mental disorders such as rabbid.,] Safety over the nature of the disease (i.e. not being a mental illness) could be very comforting and all that is needed. The combination of this and the scheduled blinking, intermittent closing and eye opening have been reported as useful.[] The best solution is to find effective treatment of eye disorder because CBS has been reported to go back with effective treatment of the cause of visual loss and improvement of visual acuity.[,] Here is a case report from a patient managed by the authors' team. Case report Approximately 85 years of age, Mr. IA had been managed by bilateral glaucoma at the Ocular Clinic of the University of Ilorin's Teaching Hospital (UITH), Nigeria for about 7 years. He had been clinically blind (without light perception) without any improvement in his visual acuity and had been in support care for more than 3 years. His 71-year-old wife had noticed that he often struck imaginary objects with his guide stick (walking weight) for which they had quarrel several times before. He was subsequently reported to one of the sons, a civil servants in the state capital who then thought that his father might be having a mental disorder, arranged for an appointment at the psychiatric clinic. Mr.'s complaint. IA was the perception of people's images in front of him. Although they did not speak, they showed complex bodily movements, such as dancing, eating, praying (e.g., raising hands, bowing, kneeling, etc., the Muslim way), being a Muslim. These experiences had been ongoing for about 8 weeks before the psychiatric appointment. He, occasionally, could identify the people he had known before his eyes began the problems. In a particular period he began to recognize his colleagues who died years earlier and was terrified by these vivid experiences. He had no strange experiences in other sensory modes; his memory was judged satisfactory by relationships and was, according to them, a "normal old man" apart from the loss of vision and recent events. The patient had no other medical complaints. Although hypertensive, it was reported that blood pressure was under good control. All the time the night dream had been satisfactory and the dream seemed to be a period of relief from the visual experiences. It does not take alcohol or other substance abuse. He had no history of mental illness. In the review, Mr. IA spoke rationally unhindered by his experiences he described in a surprising way: Complex visual upheaval in a state of clear consciousness. He was eutymic without perceptive anomalies at the time of the examination that the patient described as the usual pattern when the objects of his hallucination could disappear momentarily and re-appear. His memory was good and recognized his experiences as "false" though with terrifying potential. Physical tests were essentially normal for your age. Dry bilateral macular degeneration, pale optical disk with a cup to discal asymmetry more than 0.4 bilaterally recorded in fundoscopic. Other neurological examinations were satisfactory. Hematological and biochemical conclusions were satisfactory. It was reassured from the false nature of the visual experiences after explanations that it had no mental illness and that the problem could disappear. He was taught to keep the images away by closing his eyes sometimes and flashing repeated. Family members were educated about the nature of CBS and the importance of not ascribeing it to mental illness and not harming the situation to its disadvantage. This behavioral method was explained to the understanding of the patient and his family and regular appointment programmed to monitor the compliance and effectiveness of the method. The 2 initial weekly visits were later reduced to 4 and later 6 weekly. During these periods there was no improvement in their visual acuity, but the visual experiences had disappeared 6 months later without using any medication. Discussion There are many definitions of CBS. Our definition of CBS in this report emphasizes eye disease or visual pathways, with the phenomenology of hallucinations described by Charles Bonnet himself.[,] CBS is benign and common. However, his poor report for the afflicted, his family and even practitioners has not helped in the epidemiology of CBS. Visual loss or deprivation seems to be the prerequisite for developing CBS.[] Spontaneous CBS regression occurs for a short period of time in some patients, whereas most of them may last years.[] Although it has been reported that specific Serotonin Reuptake (ISRI) and anti-epileptic inhibitors are useful, each case must be managed according to the presentation.[] A clear case of Comorbid depression would definitely justify the use of antidepressants. In this case the patient met the criteria for Charles Bonnet and only reassurances and behavioral approaches were employed. In conclusion, doctors and family members are advised to find hallucinatory experiences by asking visually impaired people. To do this would be a long way to alleviate the suffering of the visually impaired of this syndrome that could be fainted as a mental disorder. It would also strengthen the liaison services for consultations between psychiatry and ophthalmology. FootnotesSource of support: Nil. Conflict of Interest: None declared. ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
Charles Bonnet Syndrome - The American Society of Retina Specialists

Charles Bonnet Syndrome in a Nonagenarian | Population Health Learning Network
That's Real?!? - Charles Bonnet Syndrome - Precision Family Eye Care
Visual Hallucinations: Charles Bonnet Syndrome - The Western Journal of Emergency Medicine

Charles Bonnet Syndrome in a Nonagenarian | Population Health Learning Network
Blog Therapy, Therapy, Therapy Blog, Blogging Therapy, Therapy,..

Charles Bonnet syndrome: Successful treatment of visual hallucinations due to vision loss with Yi-gan san | Semantic Scholar
PDF) Hallucinations Experienced by Visually Impaired: Charles Bonnet Syndrome
Quick Facts and Management of Charles Bonnet Syndrome

Charles Bonnet Syndrome | The Canadian Association of Optometrists
PDF) Charles Bonnet Syndrome: Successful treatment of visual hallucinations due to vision loss with selective serotonin reuptake inhibitors

When Blindness Induces Hallucinations

Charles Bonnet Syndrome: Visual Hallucinations Are My Constant Companions by VisionAware Peer Advisor Sheila Rousey - VisionAware

Charles Bonnet syndrome (CBS) – MEDsphere

The Theatre of the Mind - living with Charles Bonnet Syndrome - Henshaws

Negative outcome Charles Bonnet Syndrome | British Journal of Ophthalmology
charles bonnet syndrome
charles bonnet syndrome
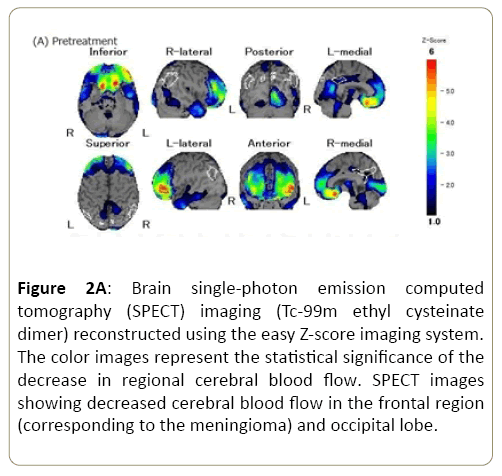
A Case Report of Yi-Gan San for the Treatment of Visual Hallucinations in a Patient with Charles Bonnet Syndrome Secondary Due to a Meningioma | Insight Medical Publishing

55 Charles bonnet syndrome ideas | syndrome, charles, bonnets
Visual Hallucinations? It Could Be Charles Bonnet Syndrome. - Germantown, Collierville, Cordova, TN

Charles Bonnet Syndrome - The American Society of Retina Specialists
Charles Bonnet Syndrome disease: Malacards - Research Articles, Drugs, Genes, Clinical Trials

P01-376 - Charles bonnet syndrome (CBS): Successful treatment of visual hallucinations due to vision loss with trazodone in three cases - ScienceDirect

The Health Hub: Charles Bonnet syndrome
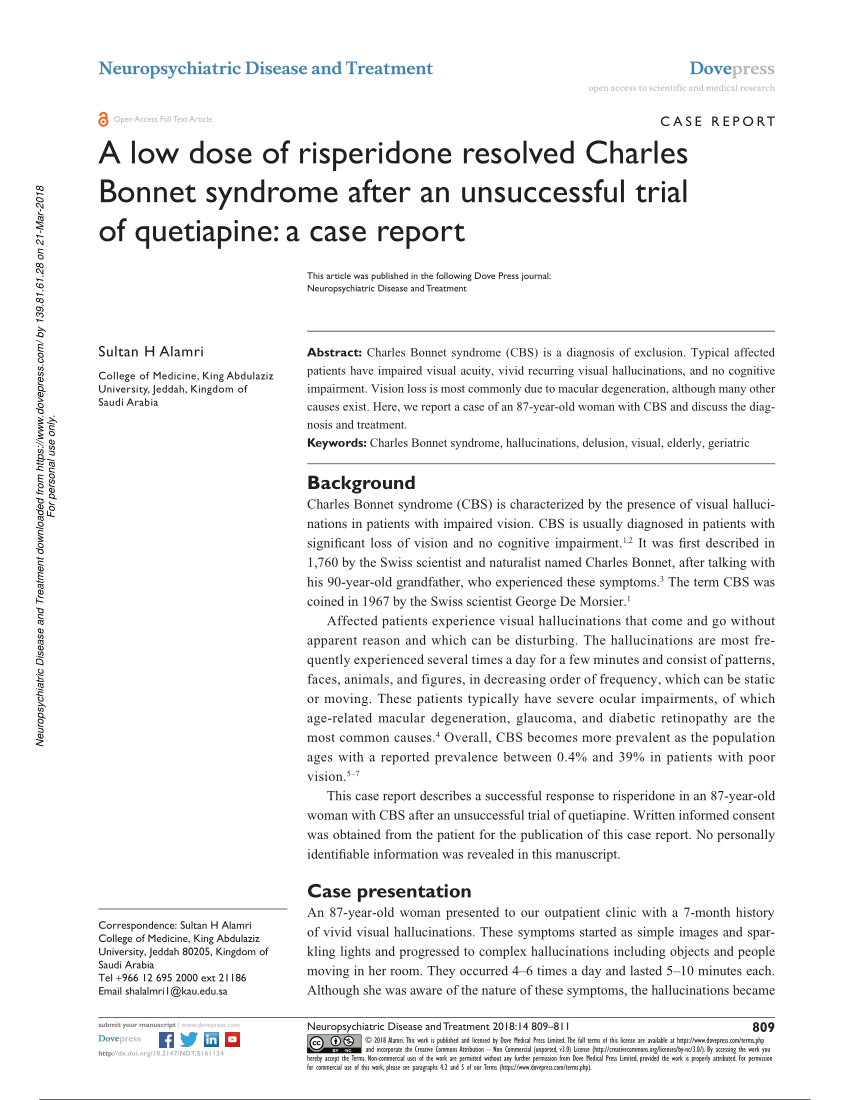
PDF) A low dose of risperidone resolved Charles Bonnet syndrome after an unsuccessful trial of quetiapine: a case report

Charles Bonnet Syndrome: what is this mysteriously underreported condition? | Vision Direct UK
Charles Bonnet Syndrome - An Unusual Macular Degeneration Symptom
What Is Charles Bonnet Syndrome? - American Academy of Ophthalmology
/https://www.thestar.com/content/dam/thestar/life/health_wellness/2016/02/24/1-in-5-with-vision-loss-see-vivid-hallucinations-canadian-study-says/cnib-study3.jpg)
1 in 5 with vision loss see vivid hallucinations, Canadian study says | The Star
Frightening visual hallucinations: atypical presentation of Charles Bonnet syndrome triggered by the Black Saturday bushfires | The Medical Journal of Australia

What is Charles Bonnet syndrome, the eye condition that causes hallucinations?

Charles Bonnet Syndrome

Charles Bonnet syndrome causes, symptoms, diagnosis & treatment
Charles Bonnet Syndrome: Evidence for a Generative Model in the Cortex?
Charles Bonnet syndrome successfully treated with levetiracetam | SpringerLink
What is Charles Bonnet syndrome, the eye condition that causes hallucinations?
Charles Bonnet Syndrome Management

PDF) Charles Bonnet Syndrome - Case series
Charles Bonnet Syndrome | theindependentbd.com
Posting Komentar untuk "charles bonnet syndrome treatment"