crohn's disease and skin boils
 Crohn's Disease Rash: Pictures, Symptoms, and More
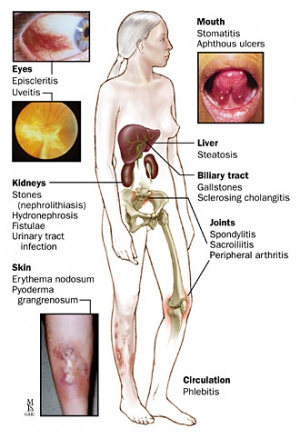
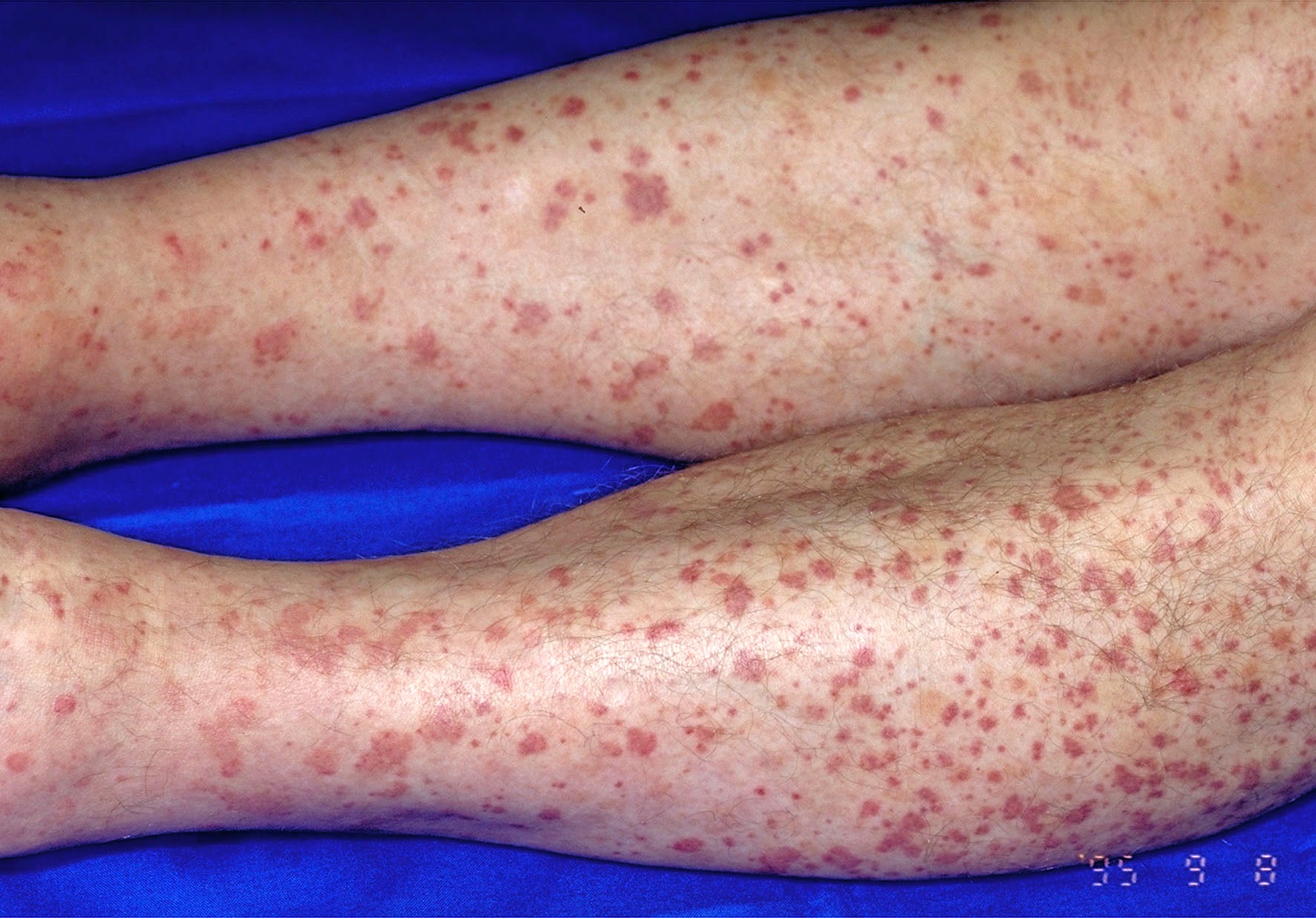
Crohn's Disease Rash: Pictures, Symptoms, and MoreWarning: The NCBI website requires JavaScript to operate. inflammatory bowel disease of suppurative hydrantitis: An unusual but existing associationCorrespondence to: Dr. Enzo Ierardi, Professor, Gastroenterology Section, Department of Emergency and Organ Transplantation, University of Bari, 70124 Bari, Italy. Phone: +39-80-5594034 Fax: +39-80-5593088AbstractIntestinal inflammatory disease (IBD) may be associated with several extra-intestinal manifestations (EIMs) involving musculoskeletal systems, hepatopancreatobiliary, ocular, kidney and lung systems, as well as skin. In recent years, suppurative hydrantitis (HS) is gaining a growing interest. IBD, especially Crohn's disease (CD), is one of the most reported associated diseases in patients with SCH. The aim of this document is to give a brief overview of the data that show a possible epidemiological and pathogenetic association between IBD and HS. We performed a combined data analysis of four studies and the prevalence of HS in patients with IBD was 12.8 per cent, with 95% BB of 11.7%-13.9%. HS was present in 17.3% of subjects with CD (95%CI: 15.5%-19.1%) and 8.5% of patients with CCU (95%CI: 7.0%-9.9%). Some elements, especially altered inmunitary imbalances, are generally involved in the pathogenesis of IBD, as well as invoked by HS. Smoking is one of the most relevant risk factors for both disorders, representing a predictor of their severity, even though there is actually a lack of studies that analyze a possible shared pathway. A role has been assumed for inheritance in the HS and the pathogenesis of the CD. Although genetic susceptibility has been demonstrated for both diseases, more studies are needed to investigate a mutual genetic route. Although the pathogenesis of IBD and HS is usually linked to immune response alterations, recent findings suggest a role for intestinal microbiota and skin, respectively. In detail, the frequent finding of Staphylococcus aureus and coagulase-negative stafilococci in cutaneous lesions of SH suggests a bacterial involvement in the pathogenesis of the disease. In addition, the microflora varies in the different skin regions of the body and, consequently, two different profiles of patients with SCH have been identified in these bases. On the other hand, it is well known that the intestinal microbiota can be considered as "the explosive mixture" at the origin of the IBD despite the fact that the exact relationship has not yet been completely clarified. A better understanding of the role of some bacterial species in the pathogenesis of IBD can be essential to developing appropriate management strategies in the near future. A final point is represented by some similarities in the therapeutic management of HS and IBD, as they can be controlled by immunomodulatory drugs. In conclusion, unregulated inflammation can cause typical HS and IBD injuries, especially when they coexist. However, this remains a largely unexploded field. Basic Council: This topic describes the main data regarding a possible association between suppurative hydroadenitis and intestinal inflammatory disease with special attention to epidemiology, etiopathogenetic factors, genetic susceptibility, intestinal microbiota/skin and therapeutic analogies. Finally, unregulated inflammation leading to microscopic granulomatous wounds can cause typical injuries of both diseases, especially when they coexist. However, this is still a largely unexplored field, and new studies are required. INTRODUCTIONIntestinal inflammatory disease (IBD) is a group of chronic inflammatory conditions of the digestive tract, which are mainly represented by Crohn's disease (CD) and ulcerative colitis (UC)[]. These disorders may be associated with several extra-intestinal manifestations (EIM) involving musculoskeletal systems, hepatopancreatobiliary, eye, kidney and lung, as well as skin. In particular, joint, liver, eye and skin EIMs are considered to be the most relevant and frequent manifestations.[] Joint participation is the most common IBD EIM[] and includes peripheral arthropathy, subclassified in pathuciarticular, polyarticular and axial arthropathy, such as sacroileitis and spondylitis. Primary sclerosing colangitis represents the most common cause of hepatobiliary involvement in patients with IBD, especially in UC[,]. Ocular complications, including episcleritis, scleritis, and uveitis, occur most often in patients with small isolated bowel CD[]. Different dermatological manifestations may arise during the course of the IBD. In fact, the pyoderma gangrenosum, psoriasis, Sweet syndrome, aftous stomatitis can be observed, even if erythema nodosum represents the most common dermatological disease associated with IBD. In addition, in recent years, suppurative hydroadenitis (HS) has been acquiring increasing interest, although it can often be misdiagnosed as a result of insufficient experience.[] The HS[] is defined as "a chronic, recurrent and debilitating inflammatory disease of follicular skin that usually presents after puberty with painful inflammatory lesions in the apocrine areas of the gland-apocrine that are carriers of the body, more commonly the axie, inguinal and anogenital regions"[]. The diagnosis of HS is based on the following clinical criteria: (1) the presence of typical lesions, (2) their characteristic places, and (3) the chronic course of the disease, showing recurrent bengalas[]. Hurley's classification identifies three progressive stages of severity of the disease: (1) the formation of abscess, individual or multiple, without the sinus tract and scarring; (2) recurrent abscesses, with formation of the tract and healing wound, as well as individual or multiple lesions widely separated; and (3) disseminated or multiple interconnected and abscessed paths throughout the area[]. IBD, especially the CD, is one of the most reported wild diseases in patients with SH[]. Patients with HS and CD have been found more often as smokers, and more likely to develop perianal diseases, and show a greater need for immunosuppressants and surgical resection.[] Moreover, based on recent evidence supporting the role of the immune imbalance in both conditions [-,-], a shared pathogen between IBD and HS can be presumed. In fact, multiple predisposing factors could influence the appearance and progression of both diseases, i.e., intestinal luminal agents, genetics and environmental factors[]. The aim of this document is to give a brief overview of the data that show a possible epidemiological and pathogenetic association between IBD and HS. EPIDEMIOLOGY AND POOLED-DATA ANALYSIS OF LITERATURE The first series of patients with CD and HS was described by Church et al[]. Twenty-four patients were recruited. The diagnosis of CD pre-dated HS for an average of 3.5 years. More recently, 15 other patients with CD and HS have been reported at the Mt. Sinai Medical Center in the period 2003-2013[]. Apart from these few cohort studies, only IBD-HS association case reports have been published. These individual cases are summarized in the [-] table. #### ###################################################### Currently, the prevalence of HS in IBD has been investigated in four studies[-]. In the pilot[], 158 patients with IBD were asked for a standardized questionnaire on the presence of suggestive symptoms of HS, such as recurrent painful boils in the armpit and/or groin.[] In addition, patients were shown an image that represented a classic HS skin injury to have a visual comparison with the injury they were suffering from. Based on this method, a prevalence of HS 16% was detected in patients with DII (17% and 14% in CDs and in patients with CAC, respectively). The same authors replicated this study in a larger sample (1093 patients with IBD), with a global prevalence of 23%, in detail 26.3% for CD and 18.3% for UC[]. A female predominance and a correlation between smoking and severe HS course were recorded. More recently, two other epidemiological studies were conducted. In a cohort study conducted in Olmsted County in Minnesota[], 679 IBD patients were followed for an average period of 19.8 years. In such patients, the clinical diagnosis of HS was established directly by dermatologists. HS was found in 8 patients (1.8 per cent), 5 with CD and 3 with UC. A significant association with obesity, female sex and perianal CD disease was found. Two out of three subjects with UC had suffered ileal anastomosis from the pouch. Compared to the control group, the incidence rate of HS in IBD was 8.9 [95 per cent confidence interval (CI): 3.6-17.5]. The cumulative incidence of 10 and 30 years of HS was 0.85% and 1.55%, respectively. Axillae, English and thighs were the most common places of participation. Finally, Janse et al[] showed a prevalence of HS of 10.6% (134 out of 1260) in their cohort of DII, with a higher association with CD (15.1%) than with UC (6.1%). In this study, the diagnosis was achieved using a validated questionnaire for HS[]. We perform a combined data analysis of the four studies cited, as shown in Figure . The prevalence of HS in patients with IBD was 12.8%, with 95% of 11.7%-13.9%. HS was present in 17.3% of CD subjects (95%CI: 15.5%-19.1%) and 8.5% of CCU patients (95%CI: 7.0%-9.9%), thus confirming a stronger CD association. In three out of four studies, the diagnosis of HS was established by a questionnaire, and these three studies showed the highest prevalence rates. This detail can lead to the conclusion that such a diagnostic strategy, despite being validated, could overestimate the prevalence of SCH compared to direct clinical evaluation. Analysis of grouped data of studies that explore the prevalence of suppurative hydrodenitis in subjects with inflammatory bowel disease (A), either Crohn's disease (B) and ulcerative colitis (C). CD: Crohn's disease; IBD: Inflammatory bowel disease; HS: Suppurative hydrodenitis. The clinical pattern of the IBD-HS association appears to be characterized by female predominance, greater frequency of smoking and by the fact that the intestinal disease prevents the involvement of the skin. The clinical and pathogenetic characteristics of the HS and IBD association are summarized in the table. Table 2Main clinical characteristics and pathogenesis of suppurative hydroadenitis and inflammatory bowel disease (adaptado de van der Zee et al[])CDUCHSLocationIntire the food tractColónInverses areas of the skinLayer of inflammation TransmuralMucosa^Deep dermatographyConfluence of lesionsNo improvement YesF Response to anti-TNFα therapyYesYesYesSyCD: Crohn's disease; UC: ulcerative colitis; HS: suppurative hydrodenitis; TNFα: Alpha tumor necrosis factor. PATHOGENETIC FACTORS HS pathogenesis remains dark. The increasing attention has focused on the role of the immune system, and recent findings suggest the involvement of the interleukin track (IL)-23/Th17 in the inflammatory response related to the SCH[]. HS is characterized by epidermal alterations such as psoriasiform epidermal hyperplasia and keratin plugs. In SH lesions, epidermis is an active source of pro-inflammatory cytokines. An inflammatory trigger and can be stimulated by IL-17+ cells. The inflammatory process in HS involves the recruitment of innate immune cells, particularly neutrophils that express IL-17[]. Notch's signaling has been proposed to be a crucial HS-pahomecism, capable of compromising the apocrine gland's homoeostasis and leading to the subsequent stimulation of TLR-mediated innate immunity.[] This mechanism has been hypothesized not only as an inducer of inflammation in the HS, but also as responsible for an insufficient regulation of feedback of over-stimulated innate immunity, linking HS to other comorbidities driven by Th17. On the other hand, an alteration of the immune imbalance with a prevalence of inflammatory cytokines for the inflammatory bowel disease has been clearly manifested and, for the time being, the therapeutic approach is strongly affected.[-] Some articles, usually involved in the pathogenesis of IBD, are also invoked for HS. Smoking is one of the most relevant risk factors for both HS and CD, representing a predictor of its severity[,]. In a recent meta-analysis containing 33 cohort studies[], CD smoking patients showed greater risks of bengall disease activity [Dód ratio (OR) = 1.97; 95% CI: 1.21-2.01], post-surgical bengalls (OR = 1.97; 95% CI: 1.36-2.85), need of both first surgeries (OR = 1.68-2. In addition, smoking has been reported as a risk factor well established in the HS by the European S1 guidelines for the treatment of reverse HS/acne[]. An association was found between the prevalence of HS and the current smoking in a French cohort comprising about 10,000 subjects (OR = 12.55; 95% CI: 8.58-18.38). This association was not demonstrated in ex-smokers[]. Despite this evidence, some aspects of the correlation between HS gravity and smoking remain controversial. In fact, Sartorius et al[] showed a more severe course in active smokers compared to non-smokers (P=.03), although no statistical difference was observed with ex-smokers. On the contrary, no smoking effect was found in the severity of the disease in a cohort study that closed 268 SH patients.[] Although the relationship between smoking and both diseases is supported by testing, a hypothetical shared pathogenetic mechanism remains unclear and can be different for HS and CD. In fact, nicotine can act in the HS by multiple pathways, i.e. overstimulation of the sweat gland with a possible obstruction of ducts and the consequent inflammation, the neurotrophil chemotaxis, the overexpression of the tumor necrosis factor (TNF) alpha in keratinocytes and the thickening of epidermidis by non neuronal acetalcoline. Simultaneously, in CD nicotine it determines a more aggressive pattern of disease, probably causing microvessel ischemia, due to the implementation of carbon monoxide concentration, and decreasing the expression of anti-inflammatory cytokines[]. Finally, the cessation of smoking improves the CD course, however this issue has not been largely investigated in the HS[]. On the other hand, it is well known that smoking does not affect the UC course. In detail, nicotine can modulate the immune system by joining the nicotine receptor acetylcholine α7 subunit expressed in macrophagus, which leads to a reduction of TNF-alpha and inflammation.[] In conclusion, even if smoking represents a crucial pathogen for both the CD and the HS, there is currently a lack of studies that analyze a possible shared pathway. Genetic Susceptibility A role for inheritance has been assumed in the HS and the pathogenesis of the CD. Up to 40% of patients with HS show a family history and a dominant autosomal pattern of inheritance has been observed in some family cases.[] Two loci in chromosome 6 and 19, and another in chromosome 1 (1p21.1-1q25.3) have been related to HS[,]. However, a recent report by Al-Ali and others did not report any association between locus 1p21.1-1q25.3 and this disease. Furthermore, mutations involving presenilin-1 genes (PSEN1), preseniline-2 enhancer (PSEN) and nicastrine (NCSTN), which determine the inactivation of the gamma-secretase enzyme complex, have also been related to HS. The mutation of this enzyme complex is involved in HS pathogenesis through aberrant triquilemmal keratinization[,-]. As for the CD, the domain of oligomerization contained in the gene 2 (NOD2) has been described as a possible hereditary factor. Three different mutations have been identified in Caucasian CD patients: a mutation of incrimination and two mutations of indicia[,]. This gene is involved in intestinal homeostasis by detecting peptidoglycan released from the intestinal microbiota and leading a mediated inflammatory response of the nuclear-κB factor (NF-κB). The alteration of this process is supposed to play a role in the development of chronic intestinal inflammation[]. A recent study by Janse et al[] sought to identify a genetic link between HS and CD. The authors evaluated three different genes, i.e., elongase elongase elongase elongase 7 (ELOVL7) gene in chromosome 5, sulfotransferase 1B member 1B (SULT1B1) and 1E member family sulfotransferase 1(SULT1E1) genes in chromosome 4. These genes on chromosome 4 originate from the sulfotransferase family, encoding enzymes that catalyze the sulfate conjugation of hormones, drugs, neurotransmitters and xenobiotic compounds. SULT1E1 encodes for an enzyme that regulates estrogen homeostasis[]. These hormones seem to be involved in the HS clinical course. In fact, the reactivation of the disease usually occurs during hypoestrogenic states, so estrogens seem to play a protective role.[] Moreover, since adiposity is another supposed risk factor for HS, the expression of SULT1E1 in the abdominal subcutaneous tissue of obese people can be considered more evidence of the role of obesity[]. In addition, Ahima et al[] showed coexpression of estrogen sulfotransferase and TNF-alpha in abdominal adipose tissue of obese subjects. This last pro-inflammatory cytokine has a role in the pathogenicity of HS and CD, as well as representing a therapeutic goal for both diseases[]. However, more studies are needed to investigate the genetic association between HS and CD. Microbiota Although the pathogenesis of IBD and HS is generally linked to immune response alterations[,], recent findings suggest a role for intestinal microbiota and skin, respectively[,]. The frequent finding of Staphylococcus aureus (S. aureus) and staphylococci (CoNS) of coagulase in cutaneous lesions of SH suggests a bacterial involvement in the pathogenesis of the disease[]. Kurzen et al[] assume that nicotine can stimulate the growth of S. aureus. Jemec et al[] suggested that S. aureus could induce the initial development process of HS, as it influences a number of anatomical alterations in capillary follicles facilitating inflammation and necrosis. CoNS, in particular Staphylococcus epidermidis (S. epidermidis), are usually non-pathogenic microorganisms and normal skin flora comas.[] Lapins et al[] found CoNS in 21 patients with HS. Sixteen of the 21 patients showed CNS at the deep levels of the skin, and in 9 of them CNS was the only isolated bacteria, thus presuming a promotional activity for these germs in the inflammation of the SCH. A retrospective histologic study analyzing 27 patients with S. showed the presence of biofilm related to S. epidermidis (i.e. an extracellular matrix used by bacteria as a protective cover against amphibian defense mechanisms and antimicrobial agents) in a fifth of the samples located in capillary follicles and sinus tracts[]. Since the microflora varies in the different skin regions of the body, in relation to different distributions of follicles and capillary glands, two different profiles of patients of SCH have been identified in a recent report by Guet-Revillet et al[]. Staphylococococcus lugdunensis was cultivated since 58% of HS lesions, which were almost exclusively Hurley's lesions in stage 1 and more frequently located in the glotopes and boobs, while a polymicrobial flora (stricken aerobics and/or aerobic actinomyotics and/or streptococci of the predominantly antibiotic group) In this sense, both the subject and the oral administrations act by killing affected bacteria and determining indirect immunomodulation with reduction of pro-inflammatory cytokines and induction of neutrophin apoptosis[]. Regarding the pathogenesis of the IBD, the modification of the intestinal microflora has been proposed, including about 1000 bacterial species, as a promotional factor. In addition, different bacterial compositions affect different sites of inflammation of the digestive system in animal models[]. In fact, in the germ IL-10-/-germ free mice, the bacterial colonization of Escheria coli or Bilophila wadworthia led to the participation of cecum or distal colon, respectively[]. Couturier-Maillard et al[] described a possible link between genetic factors and microbiome modulation. They transplanted fecal microbiota from wild-type healthy mice to poor NOD2, obtaining a risk reduction of IBD. On the contrary, the risk of disease increased in wild mice that received fecal microbiote from the poor NOD2. Smoking, as described above for HS, could determine microbiota alterations, also in the intestine with a reduction of Firmicutes and Actinobacteria and an increase in Proteobacteria and Bacteroides[,]. Modulation of the intestinal microbiota is a potential therapeutic objective in IBD and antibiotics, such as metronidazole and ciprofloxacin, which are currently used in Crohn colitis, ileocolitis and pouchitis[,]. However, tetracyclines, antibiotics used to a large extent for HS, showed a risk relationship for the development of IBD, for any exposure to these drugs, of 1.39 (95%CI: 1.02-1.90) even if no clear explanation of the mechanism was found.[] In addition, a meta-analysis[] of 11 observational studies, including 7208 patients with IBD, showed an OD of 1.57 (95%CI: 1.27-1.94) for the development of IBD after exposure to any antibiotic. This risk was higher for the CD (OR = 1.74; 95%CI: 1.35-2.23), metronidazole (OR = 5.01.95CI: 1.65-15.25), fluoroquinolls (OR = 1.79.95CI: 1.03-3.12) and in children (OR = 2.75; 95%CI: 1.72-4.38). Only the penicillin class was not associated with the beginning of the IBD. THERAPEUTIC ANALOGY And HS can show some similarities in therapeutic management, as they can be controlled by some immunomodulatory drugs. In fact, HS can benefit from anti-TNF-alpha biological therapy, similar to IBD. Numerous case reports have shown that infliximab improves skin lesions in patients with CD and HS[,,,,]. In these bases, patients suffering from HS have been treated outside the label with infliximab and etanercept, with a referral rate of about 35% and a decrease in the activity of HS of 50%[,]. In a systematic review of Haslund et al[], almost all patients treated with SCH experienced a positive effect. Infliximab therapy is indicated in medium-term HS and is well tolerated, reduces skin pain, decreases the severity of the disease and improves the quality of life[]. However, long-term results are quite poor. Adalimumab has recently been approved by the Food and Drug Administration for the treatment of SCH. This approval of the FDA is based on the results of two phase 3, PIONEER I and PIONEER II[-] core studies. In addition, Ustekinumab is a monoclonal antibody that selectively points to IL-12 and IL-23, which has been proposed for the treatment of IBD and HS. In an environment of 17 HS patients, Ustekinumab allowed, after 40 wk, a moderate improvement in 82% and a complete clinical response in 47%.[] A similar success rate, ranging from 46% to 65%, has been found in patients affected by the CD who did not benefit from other anti-TNF alpha biological agents.[,] Finally, other immunomodulators, such as corticosteroids and cyclosporine, have proved to be effective for HS[-], similar to IBD, thus supporting a possible link. However, the overall level of evidence for these drugs is very low, given the small number of HS patients described in literature so far and the lack of randomized controlled studies. CONCLUSIVE OBSERVATIONS IBLES and HS share a chronic inflammatory trait. Despite an association between these two conditions that have been reported only anecdotely, in recent years novel clinical investigations conducted on a large scale have shed new light on their association. The link between HS and IBD - CD in particular - could be stronger than expected. However, epidemiological data are not supported by strong basic studies. Despite some tests that have shown that immunodial disregulation, microbiota alteration, genetic factors and smoking can subjugate both diseases[,] a compelling in vivo test has not yet been found. In addition, the common therapeutic scenario described for IBD and HS could be another clue for your association. CONCLUSIONAn unregulated inflammation that leads to granulomatous microscopic wounds can cause typical injuries of both diseases, especially when they coexist. However, this remains a largely unexplored field, and further studies are required to dilute their pathogeny and possible therapeutic approaches, as well as interconnection between disorders and the resulting practical implications. In fact, even though the association between HS and IBD has been undervalued so far, our combined results show that the average prevalence of HS in IBD is 12.8%, with a peak for CD (17.3%). Therefore, an existing link between these two conditions can be argued. In these bases, a careful examination of the skin should usually be performed in patients with IBD, as the CD-HS association can be very deactivating. Therefore, early detection of HS in IBD could prevent the worsening of the skin disorder, thus avoiding the need for some toxic drugs. Footnotes Statement of interest: The authors declare no conflict of interest. Open-Access: This article is an open access article that was selected by an internal editor and reviewed by external experts. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0), which allows others to distribute, remix, adapt, build on this non-commercial work, and license its derivative works in different terms, provided that the original work is duly cited and the use is not commercial. See: http://creativecommons.org/licenses/by-nc/4.0/Peer-review initiated: March 21, 2016 First decision: March 31, 2016 Press release: May 4, 2016P- Reviewer: Actis GC, Ahluwalia NK, Capasso R, Zezos P S- Editor: Gong ZM L- Editor: A E- Editor: Wang CHReferencesFor , 8600 Rockville Pike, Bethesda MD, 20894 USA

Crohn's Disease and Skin Rash | LoveToKnow

Crohn's Disease Problems in Pictures: Recognize Symptoms and Get Them Treated

Crohn skin disease | DermNet NZ

Crohn's Disease Rash: Pictures, Symptoms, and More

Skin Problems Linked to IBD

Crohn skin disease | DermNet NZ

10 Skin Rashes Caused by Ulcerative Colitis

How Crohn's Disease Affects My Skin | Everyday Health

10 Skin Rashes Caused by Ulcerative Colitis

Cutaneous and Oral Manifestations of Inflammatory Bowel Disease | SpringerLink

Crohn's Disease Rash: Pictures, Symptoms, and More
/GettyImages-974936420-fead5d361527463a9df142b66bf9c6c0.jpg)
Celiac Disease, Gluten Sensitivity and Skin Issues

Skin Problems Linked to IBD

10 Skin Rashes Caused by Ulcerative Colitis
Crohn's Disease - Physiopedia

What Is Hidradenitis Suppurativa? Don't Ignore Those Lumps | HuffPost Canada Life

Cutaneous and Oral Manifestations of Inflammatory Bowel Disease | Abdominal Key

26 Photos That Show How Autoimmune Disease Affects the Skin | The Mighty

Skin Problems Linked to IBD

Hidradenitis suppurativa: Treatment, symptoms, and pictures

What Is Hidradenitis Suppurativa? Don't Ignore Those Lumps | HuffPost Canada Life

Crohn's Disease and Your Skin: Sores and More | Everyday Health

About Hidradenitis Suppurativa - HidraWear

Abscess - Wikipedia

Hidradenitis suppurativa (HS) - NHS

Crohn's Disease and Skin Issues: Rashes and More

Hidradenitis suppurativa: a common and burdensome, yet under-recognised, inflammatory skin disease | Postgraduate Medical Journal

Skin Problems Linked to IBD

26 Photos That Show How Autoimmune Disease Affects the Skin | The Mighty

Review of imaging technologies used in Hidradenitis Suppurativa - Elkin - 2020 - Skin Research and Technology - Wiley Online Library

Symptoms of Staph Infection | Everyday Health
9 Ulcerative Colitis Skin Rashes: Symptoms, Causes, Treatments
Hidradenitis suppurativa | DermNet NZ

Skin Problems Linked to IBD

Cutaneous and Oral Manifestations of Inflammatory Bowel Disease | Abdominal Key

About Hidradenitis Suppurativa - HidraWear
Hidradenitis suppurativa (syn. acne inversa) | Primary Care Dermatology Society | UK
What is perianal Crohn's? | Crohn's disease | IBDrelief

Teen With Multiple Boils

Boils
Posting Komentar untuk "crohn's disease and skin boils"